Benefits of Physiotherapy
Our Awesome Staff
We’ve been in business for more than 20 years offering chiropody, massage and physiotherapy treatment to patients within the town of Newmarket and surrounding areas. We pride ourselves on our approach to treatment that is 100% patient focused. Our policy has always been that for every Physio appointment, the patient is seen exclusively by a Physiotherapist for the entire visit. This ensures the patient’s comfort, movement and progress are exclusively observed by the therapist. Some clinics use physio assistants during patient visits…a strategy that sometimes frees up the Physiotherapist to see another patient or two at the same time – we believe treatment is more effective when our therapist stays with one patient for their entire visit. This allows the therapist to directly monitor patient’s progress by directly observing how the patient feels as they receive treatment and are directly accessible when invariably the patient has a question. Our goal in caring for our patients is that we treat them effectively and fast…we aim to minimize your time with us. This patient-centric approach only works if we have therapists who truly care about the patient.
We are very fortunate to have such caring staff. So much so that their care often extends beyond our four walls. Here’s an awesome example of that. Meet Fiona, one of our physios who has been with us for several years. She’s a licensed physiotherapist who also has a diploma in Mechanical Diagnosis and Therapy – a title possessed by less than 30 therapists in Canada. Fiona will be traveling to Peru (August 2018) with a team MDT trained therapists to participate in a humanitarian effort that will assemble a pop-up clinic to offer treatment to locals for several days. This program is aimed at providing quality MDT care to underserved areas around the world.
We asked Fiona a few questions about her trip.
——————————————-
——————————————-
Why did you get involved with this initiative?
I am passionate about MDT and travel – this is a great way to merge both. Being able to share my knowledge of MDT as an evidence-based approach for the benefit of underprivileged individuals is quite rewarding. At the heart of the method is how we educate patients to treat themselves to continue to self-manage their symptoms should they recur –MDT is not well known to Peruvians… the same holds true even in right here in Toronto, Canada!
Have you done any other humanitarian efforts before?
It wasn’t quite a humanitarian effort per-se, but I did travel to Iqaluit, NU in the Canadian Arctic. I arranged a leave of absence, to allow me the opportunity to work for the Government of Nunavut for six-weeks in April/May of 2017. There I was able to use MDT to assist with offering evidence-based care, while also while also significantly reducing their outpatient orthopaedic wait list.
So, this will be a lengthy trip to allow you to treat patients over an extended period of time, how are you affording it?
If you count 18+ hours of travel with three layovers, then yes it’ll be lengthy. But in reality, the trip will actually be relatively short. We are aiming that each patient will receive an assessment and follow-up visit during our time in Peru. What allows us to do this is the potential for rapid and lasting change with the use of McKenzie MDT.
- We are away for 11 days, but 2 of those are travel days (3-connections, 18+hr travel)
- We are offering a 3-hour workshop for local physicians and physiotherapists
- We are offering a 4-day clinic for the under-privileged
- Then, for our own fun/reward, we’ll visit Machu Picchu
Are you going with a big team?
This year will mark the largest group of clinicians gathered together for Mechanical Care Everywhere. A total of 11 of us from four different countries will participate. While those numbers appears relatively small, eight of those clinicians participating are Diploma Level. That’s amazing! But let me put it into perspective: To date there are 450 Diploma Level clinicians worldwide…eight of them will be represented on this trip! Within Canada there are 30 Diploma Level clinicians…York Rehab has 2 of them!
Why choose Peru as the destination?
Jason Ward (PT), the founder of Mechanical Care Everywhere has visited this area before and has connections there to assist with an effort of this magnitude.
It’s probably going to be an expensive trip – who is sponsoring you guys?
None of the participants received any funding for this trip – we have all paid out of our own pocket for air travel, accommodation, food and the costs associated with the 4-day clinic. Friends, family members, colleagues and various branches of the McKenzie Institute International have provided donations to Mechanical Care Everywhere to assist with offsetting some costs like the following:
- $25.00 (1 patient exam & home program)
- $50.00 (1/2 day of translators)
- $100.00 (1/2 day of clinic operation)
- $250.00 (1 full day of clinic operation)
If you want to learn more about the project you can check out the MCE website: www.mechanicalcareforum.com/mce
So this will be a series of trips so you can do follow-up visits right?
If we return to Peru again it will be a separate initiative. For this trip, our goal is to assess each patient and complete a follow-up visit during our brief time in Peru. At the heart of the method is how we educate patients to treat themselves to continue to self-manage long after we have returned home.
How is it that MDT can offer such fast results?
Mechanical Diagnosis and Treatment (MDT) is a safe, structured and evidence-based system used to assess and treat patients. The system can be applied to the spine and/or extremities. As MDT therapists, our greatest skill lies in our assessment, where we use the information collected from how a patient feels (symptoms) and how a patient moves (mechanics) to classify them into a particular group. From there, we can then match our treatment approach with the particular classification. Patients receive a program designed specifically for them, emphasizing active involvement, education, self-management and prevention of recurrence. With continual assessment and re-assessment of the patient (often less than 6 sessions), results are achieved fast, decreasing the financial burden on patients.
Once you leave Peru, how will you know if the trip is a success?
Following our 3-hour educational workshop with the local Peruvian physicians and physiotherapists, we will offer the opportunity for those interested to observe with us during our clinic days as an added learning opportunity. Thereafter, we will also network with these clinicians to encourage their learning remotely through the many forms of social media. This way, education will continue long after we have returned home.
I’d also like to share a story of MCE Founder Jason Ward – last year he had a woman waiting in line to see him specifically. She was offered the opportunity to be assessed by one of the other therapists, but declined; content to wait for Jason himself. Jason remembered her as a patient from the previous year. This woman waited hours in line to thank Jason for his assistance the year prior. She has been continuing with her exercises since Jason’s last visit and has remained pain-free as a result. Now THAT is proof in the pudding!
——————————————-
——————————————-
Thanks for taking the time to share a bit about this initiative Fiona. Have a great trip!
We are so proud of Fiona.
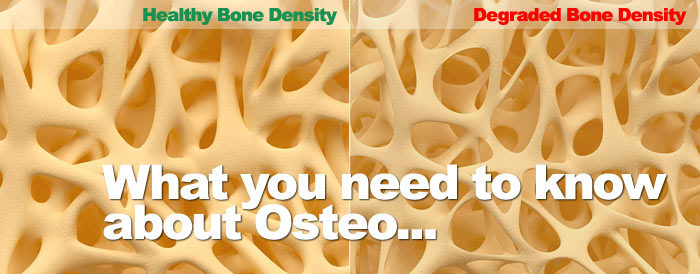
Osteoporosis – What You Need to Know
Osteoporosis is a health condition that affects bones, leading to bone thinning and loss of density, ultimately affecting their structural integrity and leading to increased fracture risk. It can occur at any age, although is more common as age increases; 1 in 4 women and 1 in 8 men over the age of 50 are affected by it. It is often called the “silent thief” because it can be present without any active symptoms. Its presence can be confirmed definitively only by a Bone Mineral Density test, which is a special type of X-ray.
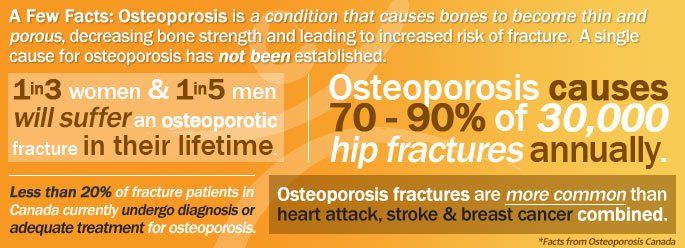
No single cause of osteoporosis has been identified. As we develop and grow through childhood and adolescence, we continue to build and “bank” bone until the age of 30. The more that we build bone during this critical period, the greater defence we have against the development of osteoporosis later in life. Bone “likes” to be exposed to regular, varying stresses to adapt and grow stronger; for example, playing soccer, which involves varying amounts of jogging, sprinting, jumping, and kicking, is an example of good stress. This means that everyone should be active from a young age and continue to remain active as they grow older to minimize the risk of osteoporosis, amongst many other health conditions – unfortunately this seems to be far from the norm.
The group at greatest risk of developing osteoporosis is post-menopausal women over the age of 50. While both men and women begin to naturally lose bone starting in their mid-30s, women lose bone at a much greater rate as they approach menopause – about 2-5% per year. This risk is even greater if they are physically inactive. This is because bone is a very active tissue with lots of turnover, the misconception is that we tend to think of it as a fixed structure. There are specialized bone cells that deconstruct it, mainly to access stored calcium for numerous bodily functions, and other specialized cells that reconstruct it as it adapts to the loads that we put on it. If we don’t put enough stress through it by moving and exercising, the reconstructing cells are insufficiently stimulated and there is a gradual loss of bone.
As mentioned above, the risk for fracture is much higher when osteoporosis is present. Areas that are most common to fracture are the spine and hip. Usually we would think that a significant trauma such as a hard fall or a car accident would be necessary to cause a fracture, but in osteoporosis much lesser forces are needed; even repetitive bending can be enough to cause a spinal fracture. Compounding this problem is that because people with osteoporosis are often less active, they do not have the same balance and strength as active people, and so are more prone to falls.
What can be done to counteract osteoporosis, or prevent it from happening in the first place? While medical interventions such as supplementary calcium and Vitamin D are important to ensure bones have the nutrients they need to remain strong, one important way to help manage your disease is through exercise. Just like muscle, bone adapts to the loads applied to it and become stronger. Our Newmarket Physiotherapy clinic has a specialized exercise program called Osteo-Circuit for those with osteoporosis or low bone density. You will be assessed by a physiotherapist to determine your suitability for the program and what your customized exercise plan should be. Inquire about the next 6 week program offered at our Newmarket Physiotherapy Clinic. Here’s to better and stronger bone health – you can do it!
Is Chronic Pain something you live with forever? The Answer may surprise you.
Do you have a bum shoulder? A bad knee? Do you have a pain from an injury that has persisted for months or years? You may have talked to friends or co-workers about it and likely heard “Oh that’s chronic pain and it’s something you just live with” or “Well, what do you expect, you’re getting older”. Many people who develop such pains assume that because their injury was a long time ago, their pain is set in stone and there’s nothing you can do about it. Or, as you get older, it will be more difficult to get rid of it. Well, there is hope! These long-lasting pains don’t have to stay around forever; there are several courses of recovery that can take place depending on the nature of the original injury and the natural repair process that has taken place since.
In scenario 1, let’s assume you have pain from an old shoulder injury. It got better initially but just didn’t seem to fully heal, and now you’re left with some lingering pain. Normally what happens during the first few weeks of soft tissue healing (for example with muscle or ligament) is your body deposits scar tissue to rebuild the injured site. If we looked at the tissue fibres under a microscope at this point we would find them disorganized and unlike the original tissue where the fibres are lined up in parallel. If controlled stress (stretching and/or strengthening) is applied to the injured site at this stage, it would begin to remodel and look more like the original tissue. Depending on the severity of the original injury and assuming no other complications, after several more weeks of recovery and exercise the injured site can become pain-free and function well.
However, some people mistakenly believe that a tissue will heal fully on its own with time, or initially they misinterpret the pain that occurs with stressing the injured site and avoid it. In both cases, the remodelling process is not undertaken, and the scar tissue remains disorganized and tight, causing pain every time it is stressed. The good news is if you understand what is happening and are guided through the remodelling process with the assistance of a physiotherapist, you can make changes to this tissue and achieve a gradual recovery over several weeks or months. Typically this will involve an individualized and structured home exercise program – which can involve strengthening and stretching.
In scenario 2, let’s say you find yourself with pain from an old knee injury and no matter how much you try to remodel it following the principles above, the pain doesn’t go away. Sometimes what can happen at the time of injury is the resting position of the joint is disturbed so now it isn’t “hinging” properly anymore. Again, the positive here is this situation can be reversed quickly with the help of a physiotherapist who can identify the right movements to return it to its proper position. It’s like a floor rug being ruffled up in front of a door – when you try to open the door, it gets blocked by the rug. So what you have to do is find the right way to move the rug and then the door will open smoothly again. There are cases where pain that has persisted for years can respond to simple movements rapidly due to this problem.
The bottom line is this: just because you have had pain for months or years from an old injury that seems to be unchanging, it doesn’t mean you’re doomed to live with it. There’s hope! You can simply start by making an appointment with a physiotherapist. They’ll listen to you and do a thorough assessment to determine the nature of the problem, and design a recovery plan for you. Remember, you don’t need a doctor’s referral to book an appointment with a physiotherapist. As long as you’re willing to put in the effort to recover, the results will likely follow. Wouldn’t it be nice to leave behind that nagging pain you thought would be with you for the rest of your life?
Exact Same Knee Pain…Different Causes
When you’re told you need to go see a physiotherapist, what do you think of? You may think of stretching, strengthening, heat/ice, ultrasound, endurance training, balance exercises, or electrical stimulation. All these thoughts fall under the category of treatment. What you may not consider is your physiotherapist as a diagnostician. Therapists who are trained in Mechanical Diagnosis & Therapy, also known as the McKenzie Method, are diagnosticians first and foremost. The three cases presented below illustrate this point – all three patients came in with pain in the front of their knees, but the underlying reason for each pain was different and demanded unique management strategies.
The first patient was a 14-year-old female who had right knee pain episodically for the past 2 years – at the time of assessment she had it for 1 month. It was painful when bending, standing, squatting, lunging, and sometimes when sitting, walking, and negotiating stairs, and prevented her from participating in karate. The history and physical exam indicated it could be a typical knee problem, but in the McKenzie Method the lumbar spine (lower back) is first assessed for any contribution – spinal conditions can refer in unusual ways to the extremity. Ultimately it was found that repetitive lumbar extension brought about relief from her knee pain, which she was easily able to do at home, and after some reconditioning exercises, she made a full return to karate.
The second patient was a 60-year-old male who had pain in both knees for a year after a day of heavy ladder use at work. The pain was there mostly when getting out of a chair and walking the first few steps, and also sometimes with squatting. As with the patient above, his lower back was assessed for any contribution and was ruled out because of no change to his presentation. His knees were then assessed with repetitive movement testing. Repetitive straightening (hyperextension) caused a significant reduction in his squatting pain. Within a week of performing this exercise 4-5 times per day, he was 90% free of pain with full movement and strength.
The third patient was a 39-year-old male who had right knee pain intermittently for 2 years after doing some moving; going up and down stairs and squatting were his two most painful activities. As above, his lumbar spine was assessed first, which had no effect on his presentation, so it was ruled out. Repeated knee movements also had no lasting effect but it was found that repetitive straightening of his knee with an ankle weight consistently produced his pain. This pain did not remain afterward. This presentation is consistent with a dysfunction or suboptimal healing of the patellar tendon. Consistent remodeling of his tendon via progressive resistance exercises over two months proved to steadily diminish his pain. He was able to go up and down stairs without pain at that point and had made a return to biking.
The three cases outlined above all had frontal knee pain, but for different reasons: one was due to a lower back joint problem, one was due to a knee joint problem, and the last was the result of a patellar tendon dysfunction. These diagnoses were sorted out following the principles of the McKenzie Method and each patient was given an effective self-management strategy that led to resolution of the problem. Make sure the next time you need to see a physiotherapist that you are given a good mechanical assessment that focuses on understanding the cause of your problem, and not just what can be done to treat the symptoms.
Our Newmarket Physiotherapy clinic has several physiotherapists trained as McKenzie Method practitioners. Our physio clinic also has 2 of only a handful of therapists in Canada who have completed the Diploma Program in Mechanical Diagnosis and Therapy (MDT) and the most number of credentialed therapists in an Ontario clinic.
The McKenzie Method – Mechanical Diagnosis & Therapy (MDT)
If you’ve ever had joint pain, this situation may be familiar to you: every family member, friend, and coworker has the time-honoured “magic solution” to get you better. Whether it’s heat, medication, meditation, or dousing yourself in honey, everyone has a suggestion. One you may have heard about is doing “McKenzie exercises” to recover. What are these exercises? Are they effective? How does it work?
“Mechanical Diagnosis & Therapy” or MDT
Also known as Mechanical Diagnosis & Therapy (MDT), the McKenzie Method is a comprehensive assessment system for orthopedic conditions such as back pain or shoulder pain, and is more than just a series of exercises. It allows the assessor to reliably classify you into different subgroups so that the right treatment can be applied. Practitioners need to understand you and your condition before they can hope to begin any treatment. It’s just like taking your car into the mechanic when something is malfunctioning – a good mechanic will take the time to ask you what the problem is (what are the symptoms?), and then will run tests to determine the source of the problem (does it hurt if you move that way?). You can’t expect the repairs to be made immediately – careful diagnosis is required first.
The McKenzie Method system was developed by New Zealand physiotherapist Robin McKenzie in the 1950s and 60s. One day he had a patient with back pain radiating down to his foot come in and he told him to go lie down on an unoccupied bed. Little did Robin know, the top half of the bed was at an angle, so the patient laid face-down on the bed with his back in maximum extension (like the cobra position in yoga). At the time the conventional wisdom was this was a terrible position for back pain. However, when Robin asked the patient how he was doing, he remarked that the leg pain had disappeared. This was so contrary to all his teachings that it inspired him to begin experimenting with different postures and movements and making careful observations with his patients. Patterns began to emerge, and he realized that these patterns could apply to all joints of the body.
McKenzie Method Today
Today the McKenzie Method is practiced globally by rehabilitation professionals of many backgrounds. Since its humble beginnings in New Zealand, it has been supported by numerous scientific publications around the world. Despite this, it is not a universally adopted system. Because the emphasis is first on understanding the problem at its root, which may take several sessions to achieve, it is at odds with the “treatment first” approach. Too often in rehabilitation the approach is to treat the symptoms with modalities such as heat or electrical stimulation, as opposed to getting an understanding of the cause. Fortunately, when the cause is identified using MDT, treatment can be very effective.
The majority of musculoskeletal problems are mechanical in nature – they are affected by movement. Mechanical problems require mechanical solutions, and often it is simply a matter of finding the right direction and force to move into. For example, a person with knee pain might respond to repeated knee straightening movements and have less pain and improved squatting mechanics as a result. If the right movement is applied regularly and aggravating factors are avoided, then rapid improvement is seen, often in a matter of days. Most people can treat themselves once they know what to do – patient independence is one of the central philosophies of MDT. This saves time and eliminates the need for long courses of treatment with many visits. Additionally, you will be shown how to prevent future episodes from occurring, and how to self-treat if the pain does happen to return.
So, the next time that shoulder starts to ache or your knee starts to lock up, instead of using the old family remedies, try looking up a certified McKenzie practitioner. The solution to your problem may be simpler than you think. York Rehab’s Newmarket Physiotherapy clinic has the most therapists certified in McKenzie treatment in Ontario.